To palliate, literally means “to cloak.” Palliation can view disapprovingly as merely covering up problems. However, as currently used in American medicine, “palliative care” is a widely accepted term for an approach to the management of a terminal illness that focuses on symptom control and support rather than cure or life prolongation.[3]
Today, healthcare includes a lot of activities ranging from prenatal to antenatal to preventive care and palliative care. Palliative care involves a variety of services delivered in support of the patient and their family, by a mix of professionals who all have equally important roles to play – including physicians, nurses, support workers, paramedics, pharmacists, physiotherapists and volunteers.
A fundamental goal of palliative care is the relief of pain and other symptoms. Successful approaches to the assessment and management of pain and some physical and psychological symptoms have been established in controlled trials [1]
Palliative care improves the quality of life of patients and that of their families who are facing challenges associated with life-
threatening illnesses, whether physical, psychological, social or spiritual. The quality of life of caregivers improves as well. Early delivery of palliative care reduces unnecessary hospital admissions and the use of health services. Each year, an estimated 56.8 million people, including 25.7 million in the last year of life, need palliative care. Unfortunately, only about 14% of people who need palliative care currently receive it. Unnecessarily restrictive regulations for morphine and other essential controlled palliative medicines deny access to adequate palliative care. [2]
The global need for palliative care is expected to grow as a result of the ageing of populations and the rising burden of non-communicable diseases and some communicable diseases. In Karamoja, one of Uganda’s poorest regions[4]. Karamoja sub-region is unquestionably disadvantaged by not just inadequate health technology but also its relative location from the better-equipped National Referral Hospital, Mulogo. Of the socio-economic nature of the people, most patients live below the poverty level. Several cancer patients in need of chemotherapy and radiotherapy are unable to access the services due to the long distance to reach the national referral hospital. Prompting the hospitals to offer the most they can, palliative care.
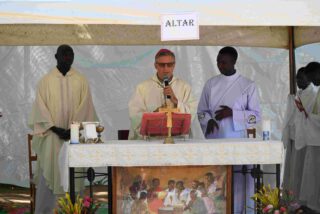
At St. Kizito Hospital Matany, palliative care is provided by Primary Health Care nurses (PHC) who travel -with the support of the Hospital- to visit the patients and give medical supplies to the homes of residents. morphine is the most prescribed and delivered.
If it was just about the medical conditions, the challenges would have been much simpler to alleviate but, financial constraints limit the patients from even getting food and water. Most of the patients visited are in visible misery arising from their inability to make a living. Considering how they have been making a living from manual labour and the incomes were hand-to-mouth, health conditions like these are just forcing the patients to live shorter than they could have.
The Primary health care team with little funding from the hospital and well-wishers have made efforts to help the patients with the basics of food and water to accompany the strong medications that demand a lot from the body. The Hospital Palliative care nurse team on several occasions have carried along some food items like posho, beans, and milk powder among others as they deliver the morphine refill for the patients during the home visits.
In one particular visit that got documented, the team visited two terminally ill cancer patients who reside in the neighbourhood of the hospital in sheer lack and agony. As narrated in the video, these two individuals are having the hospital as their only refuge and stronghold.
The first case is of 69y/f diagnosed with cervical cancer, about 5 years ago. However, she is homeless after her house collapsed earlier this year; besides the distress from the illness, shelter and food are up there on her list of needs to sustain life. She was better off during the times when she was admitted to the medical ward of Matany Hospital, at least shelter, water and even food were assured.
The second case is of an elderly woman who was diagnosed with cervical cancer in her early 40s, she has been a seamstress before her health conditions couldn’t allow her to continue with the decent living, she has been making for the past 2-3 decades. Now she sits home and hopes that the pain and hunger don’t come at once, at least one at a time -as she meditates on her demise.
When visiting such patients, one can wonder whether the delivered medication is the first on their list of priorities or another burden. It instantly evokes mixed emotions: Seeing them smile in agony when the team arrives, seeing them laugh while the joy lasts, the joy that lasts as long as the team’s company in the dry compound. While for the team members, one cannot get the thought of these visits of his/her mind: The thought of knowing you are their only balance between agony and peaceful passing on. The thought that, of all the supplies delivered, the medications are probably still there but not the food -not anymore.
Thought that you would love to offer more helping hands but as a team member of a hospital like this,
| Challenges faced by the palliative care nursing team. |
Matany Hospital also has its financial constraints. Unlike in the past, there is currently no running program for supplying food to needy patients whose ability to make a living for themselves got hindered by their health conditions.
The long distances walked by the palliative care team nurses during the home visits. The palliative nurse always walks on foot to go and visit their clients in their homes Some of these visits enable them to keep counselling the patients and also to offer them psycho-social support. Refills of analgesics and delivery of some edible items for them.
Out of utter regard for humanity, the hospital is obliged to deliver medical assistance to each one of the terminally ill patients who have been discharged to reside in their respective homes. There is a limitation on transportation; the homes near and far homes are to be visited routinely. The team members have been moving on foot to homes that are at the extreme ends -extreme ends of the walkable distance spectrum. In the instance that the home is outside this spectrum, it is probably in the range of a bicycle rider. Bicycles are used in most cases when walking the entire distance is not humanely achievable; Unfortunately, not even bicycles are readily available for palliative care nurses.
Inadequate supplies to cater for the demanding needs of palliative care patients. What the Primary Health Care team of Matany Hospital prays for is a vehicle, a vehicle strong enough to reach the deepest ends of the villages, a vehicle just accommodative enough for the team members and the supplies to be taken along. The increased poverty levels among the residents leave the majority without the capacity to access basic needs. The vehicle will further be pivotal to this service since there are patients in hospital beds that have been referred to Mulago National Referral Hospital for Chemotherapy and Radiotherapy but are unable to afford the fares. They too can get some sigh of relief and some light of hope if transportation is available.
- Morrison, R. S., & Meier, D. E. (2004). Palliative care. New England Journal of Medicine, 350(25), 2582-2590.
- World Health Organisation, 2020; Palliative care.
https://www.who.int/news-room/fact-sheets/detail/palliative-care
- Billings, J. A. (1998). What is palliative care? Journal of palliative medicine, 1(1), 73-81.
https://www.liebertpub.com/doi/pdf/10.1089/jpm.1998.1.73
- Aljazeera, 2022, Hunger killing children in a forgotten corner of Uganda.
https://www.aljazeera.com/gallery/2022/6/15/photos-hunger-killing-children-in-forgotten-corner-of-uganda